Navigating Additional Payer Challenges
These downloadable flash cards provide potential examples of other ancillary insurance issues you and your patients may encounter after you prescribe EYLEA HD.
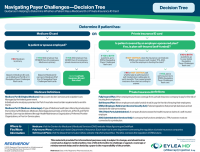
Start Here: Decision Tree
A guide to help determine whether a patient has a Medicare ID card or private insurance card.
Ancillary Flash Cards

Help Understanding ERISA
Information to help you begin to navigate potential reimbursement questions with ERISA-related claims.
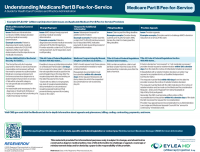
Help Understanding Medicare Part B Fee-for-Service
Potential examples of EYLEA HD claim questions and applicable provisions for patients with Medicare Part B Fee-for-Service.
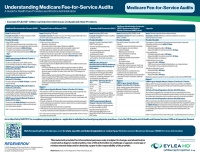
Help Understanding Medicare Fee-for-Service Audits
Potential examples of scenarios regarding questions that may occur when Medicare conducts audits of providers who bill fee-for-service programs.
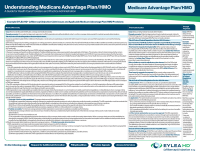
Help Understanding Medicare Advantage Plan/HMO
Potential examples of claim questions that providers and administrators may encounter after prescribing EYLEA HD for patients with Medicare Advantage.
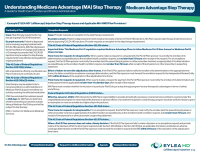
Help Understanding Medicare Advantage Step Therapy
A guide for navigating step therapy with EYLEA HD for patients with Medicare Advantage plans.

Help Understanding the Medicare Appeals Process
Potential examples of questions providers and administrators may encounter when appealing EYLEA HD through Medicare Part B and Part C.

Help Understanding Skilled Nursing Facilities (SNFs)
Potential examples of SNF-related reimbursement questions providers and administrators may encounter after prescribing EYLEA HD.
This material is provided for informational purposes only, is subject to change, and should not be construed as legal or medical advice. Use of this information to challenge or appeal a coverage or reimbursement delay and/or denial by a payer is the responsibility of the provider.
ERISA = Employee Retirement Income Security Act; HMO = health maintenance organization; ID = identification.
This material is provided for informational purposes only, is subject to change, and should not be construed as legal or medical advice. Use of this information to challenge or appeal a coverage or reimbursement delay and/or denial by a payer is the responsibility of the provider.